Happy Mother’s Day!
In honor of Mother’s Day I wanted to make my “Post a Day in May For Mental Health Awareness” about Mothers. My post today is specifically related to new mothers and postpartum depression, bipolar, PTSD, anxiety and psychosis.
I had severe postpartum depression after the birth of my first child. After being diagnosed with postpartum depression and taking the anti-depressant Prozac, I was soon diagnosed with bipolar disorder and the rest is history.
I always wanted to have children since I was ten years old and I wanted to be the best Mommy in the world. That was my dream. Little did I know when I gave birth to my first child, I would be delievered in the afterbirth of my delivery and I would never be the same again. I had no idea how drastically my life would be forever changed. This will be covered in detail in my upcoming memoir SHAME ATE MY SOUL: RISING ABOVE THE STIGMA OF MENTAL ILLNESS, SUICIDE ATTEMPTS AND ADDICTION
My mental illness life began with postpartum depression…
Postpartum Depression
The birth of a baby can trigger a jumble of powerful emotions, from excitement and joy to fear and anxiety. But it can also result in something you might not expect — depression.
Many new moms experience the “postpartum baby blues” after childbirth, which commonly include mood swings, crying spells, anxiety and difficulty sleeping. Baby blues typically begin within the first two to three days after delivery, and may last for up to two weeks.
But some new moms experience a more severe, long-lasting form of depression known as postpartum depression. Rarely, an extreme mood disorder called postpartum psychosis also may develop after childbirth.
Postpartum depression isn’t a character flaw or a weakness. Sometimes it’s simply a complication of giving birth. If you have postpartum depression, prompt treatment can help you manage your symptoms — and enjoy your baby.
Symptoms
Signs and symptoms of depression after childbirth vary, and they can range from mild to severe.
Postpartum baby blues symptoms
Signs and symptoms of baby blues — which last only a few days to a week or two after your baby is born — may include:
- Mood swings
- Anxiety
- Sadness
- Irritability
- Feeling overwhelmed
- Crying
- Reduced concentration
- Appetite problems
- Trouble sleeping
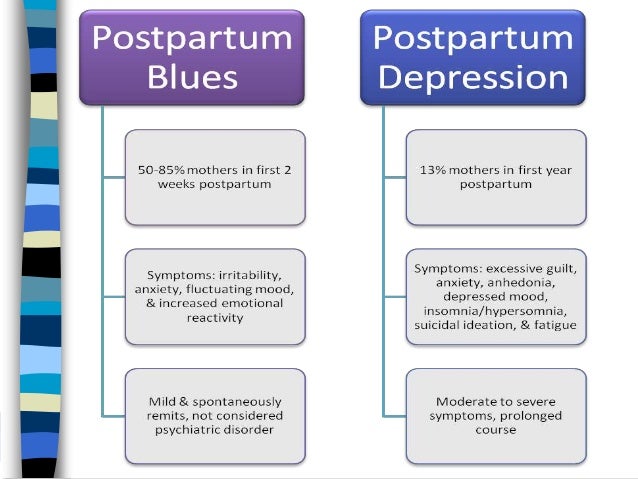
Postpartum Depression
- Postpartum depression may be mistaken for baby blues at first — but the signs and symptoms are more intense and last longer, eventually interfering with your ability to care for your baby and handle other daily tasks. Symptoms usually develop within the first few weeks after giving birth, but may begin later — up to six months after birth.
- Postpartum depression symptoms may include:
- Depressed mood or severe mood swings
- Excessive crying
- Difficulty bonding with your baby
- Withdrawing from family and friends
- Loss of appetite or eating much more than usual
- Inability to sleep (insomnia) or sleeping too much
- Overwhelming fatigue or loss of energy
- Reduced interest and pleasure in activities you used to enjoy
- Intense irritability and anger
- Fear that you’re not a good mother
- Feelings of worthlessness, shame, guilt or inadequacy
- Diminished ability to think clearly, concentrate or make decisions
- Severe anxiety and panic attacks
- Thoughts of harming yourself or your baby
- Recurrent thoughts of death or suicide
- Untreated, postpartum depression may last for many months or longer.
Postpartum Bipolar Disorder – Bipolar 1 and Bipolar 2
There are two phases of a bipolar mood disorder: the lows and the highs. The low time is clinically called depression, and the high is called mania or hypomania. Many women are diagnosed for the first time with bipolar depression or mania during pregnancy or postpartum. In Bipolar 2, the manic episode is less apparent; the highs and lows are not as extreme, and sometimes it is more apparent to friends and families than to the individual going through the phases.
The criteria for a diagnosis of a bipolar mood disorder is that the symptoms last longer than four days and interfere with functioning and relationships. Sometimes the ups and downs seem to happen at almost the same time; this confusing state is called a mixed episode. These cycles and emotional states are more than the moodiness of pregnancy or postpartum. For many women, pregnancy or postpartum might be the first time she realizes that she has bipolar mood cycles.
Sometimes, a person with severe episodes of mania or depression has psychotic symptoms too, such as hallucinations or delusions. These symptoms present a high risk and must be treated immediately. In an emergency, click here for information.
Bipolar disorder can look like a severe depression or anxiety.
In pregnant and postpartum women, a bipolar depression can look just like a very severe depression, or might be experienced as anxiety. It is very important that your mood history is reviewed to assess whether you have had times of a persistently elevated mood, decreased need for sleep, and periods of over-average productivity. There is a very high risk of increased severity if you are treated only for depression, but have the potential to move into a manic or hypomanic part of your cycle.
Bipolar I Mood Disorder
- Periods of severely depressed mood and irritability
- Mood much better than normal
- Rapid speech
- Little need for sleep
- Racing thoughts, trouble concentrating
- Continuous high energy
- Overconfidence
- Delusions (often grandiose, but including paranoid)
- Impulsiveness, poor judgment, distractibility
- Grandiose thoughts, inflated sense of self-importance
- In the most severe cases, delusions and hallucinations
Bipolar II Mood Disorder
- Periods of severe depression
- Periods when mood much better than normal
- Rapid speech
- Little need for sleep
- Racing thoughts, trouble concentrating
- Anxiety
- Irritability
- Continuous high energy
- Overconfidence
It is essential to consult an informed professional with experience and training in mental health assessment and treatment during pregnancy and postpartum. Each woman’s situation is different, but it is best practice to consult before pregnancy and to have a treatment plan in place. There is a growing body of research that explores the risk-benefit balance of using mood stabilizers during pregnancy and breastfeeding.
Please visit our page about perinatal medication resources for more information.
© Postpartum Support International – PSI

Postpartum Post-Traumatic Stress Disorder (PTSD)
Approximately 9% of women experience postpartum post-traumatic stress disorder (PTSD) following childbirth. Most often, this illness is caused by a real or perceived trauma during delivery or postpartum. These traumas could include:
- Prolapsed cord
- Unplanned C-section
- Use of vacuum extractor or forceps to deliver the baby
- Baby going to NICU
- Feelings of powerlessness, poor communication and/or lack of support and reassurance during the delivery
- Women who have experienced a previous trauma, such as rape or sexual abuse, are also at a higher risk for experiencing postpartum PTSD.
- Women who have experienced a severe physical complication or injury related to pregnancy or childbirth, such as severe postpartum hemorrhage, unexpected hysterectomy, severe preeclampsia/eclampsia, perineal trauma (3rd or 4th degree tear), or cardiac disease.
Symptoms of postpartum PTSD might include:
- Intrusive re-experiencing of a past traumatic event (which in this case may have been the childbirth itself)
- Flashbacks or nightmares
- Avoidance of stimuli associated with the event, including thoughts, feelings, people, places and details of the event
- Persistent increased arousal (irritability, difficulty sleeping, hypervigilance, exaggerated startle response)
- Anxiety and panic attacks
- Feeling a sense of unreality and detachment
Postpartum PTSD is temporary and treatable with professional help. If you feel you may be suffering from this illness, know that it is not your fault and you are not to blame. You can use our resource page to reach out now. We understand what you are going through and will connect you to people who understand and can help.
© Postpartum Support International – PSI

Postpartum Anxiety
Approximately 6% of pregnant women and 10% of postpartum women develop anxiety. Sometimes they experience anxiety alone, and sometimes they experience it in addition to depression.
Symptoms
- Constant worry
- Feeling that something bad is going to happen
- Racing thoughts
- Disturbances of sleep and appetite
- Inability to sit still
- Physical symptoms like dizziness, hot flashes, and nausea
In addition to generalized anxiety, there are some specific forms of anxiety that you should know about. One is Postpartum Panic Disorder. This is a form of anxiety with which the sufferer feels very nervous and has recurring panic attacks. During a panic attack, she may experience shortness of breath, chest pain, claustrophobia, dizziness, heart palpitations, and numbness and tingling in the extremities. Panic attacks seem to go in waves, but it is important to know that they will pass and will not hurt you.
Another form of anxiety is Postpartum Obsessive Compulsive Disorder. Learn more about it here.
Postpartum and antepartum anxiety are temporary and treatable with professional help. If you feel you may be suffering from one of these illnesses, know that it is not your fault and you are not to blame. You can use our resource page to reach out now. We understand what you are going through and will connect you to people who understand and can help.
© Postpartum Support International – PSI
Postpartum Psychosis
With postpartum psychosis — a rare condition that typically develops within the first week after delivery — the signs and symptoms are even more severe. Signs and symptoms may include:
- Confusion and disorientation
- Obsessive thoughts about your baby
- Hallucinations and delusions
- Sleep disturbances
- Paranoia
- Attempts to harm yourself or your baby
Postpartum psychosis may lead to life-threatening thoughts or behaviors and requires immediate treatment.
When to see a doctor
If you’re feeling depressed after your baby’s birth, you may be reluctant or embarrassed to admit it. But if you experience any symptoms of postpartum baby blues or postpartum depression, call your doctor and schedule an appointment. If you have symptoms that suggest you may have postpartum psychosis, get help immediately.
It’s important to call your doctor as soon as possible if the signs and symptoms of depression have any of these features:
- Don’t fade after two weeks
- Are getting worse
- Make it hard for you to care for your baby
- Make it hard to complete everyday tasks
- Include thoughts of harming yourself or your baby
If you have suicidal thoughts
If at any point you have thoughts of harming yourself or your baby, immediately seek help from your partner or loved ones in taking care of your baby and call 911 or your local emergency assistance number to get help.
Also consider these options if you’re having suicidal thoughts:
- Call your mental health specialist.
- Call a suicide hotline number — in the U.S., call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255).
- Seek help from your primary doctor or other health care provider.
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
Helping a friend or loved one
People with depression may not recognize or acknowledge that they’re depressed. They may not be aware of signs and symptoms of depression. If you suspect that a friend or loved one has postpartum depression or is developing postpartum psychosis, help them seek medical attention immediately. Don’t wait and hope for improvement.
Causes
There’s no single cause of postpartum depression, but physical and emotional issues may play a role.
- Physical changes. After childbirth, a dramatic drop in hormones (estrogen and progesterone) in your body may contribute to postpartum depression. Other hormones produced by your thyroid gland also may drop sharply — which can leave you feeling tired, sluggish and depressed.
- Emotional issues. When you’re sleep deprived and overwhelmed, you may have trouble handling even minor problems. You may be anxious about your ability to care for a newborn. You may feel less attractive, struggle with your sense of identity or feel that you’ve lost control over your life. Any of these issues can contribute to postpartum depression.
Risk factors
Postpartum depression can develop after the birth of any child, not just the first. The risk increases if:
- You have a history of depression, either during pregnancy or at other times
- You have bipolar disorder
- You had postpartum depression after a previous pregnancy
- You have family members who’ve had depression or other mood stability problems
- You’ve experienced stressful events during the past year, such as pregnancy complications, illness or job loss
- Your baby has health problems or other special needs
- You have difficulty breast-feeding
- You’re having problems in your relationship with your spouse or significant other
- You have a weak support system
- You have financial problems
- The pregnancy was unplanned or unwanted
Complications
Left untreated, postpartum depression can interfere with mother-child bonding and cause family problems.
- For mothers. Untreated postpartum depression can last for months or longer, sometimes becoming a chronic depressive disorder. Even when treated, postpartum depression increases a woman’s risk of future episodes of major depression.
- For fathers. Postpartum depression can have a ripple effect, causing emotional strain for everyone close to a new baby. When a new mother is depressed, the risk of depression in the baby’s father may also increase. And new dads are already at increased risk of depression, whether or not their partner is affected.
- For children. Children of mothers who have untreated postpartum depression are more likely to have emotional and behavioral problems, such as sleeping and eating difficulties, excessive crying, and attention-deficit/hyperactivity disorder (ADHD). Delays in language development are more common as well.
Treatments and Medications
Treatment and recovery time vary, depending on the severity of your depression and your individual needs. If you have an underactive thyroid or an underlying illness, your doctor may treat those conditions or refer you to the appropriate specialist. Your doctor also may refer you to a mental health provider.
Postpartum depression is often treated with psychotherapy (also called talk therapy or mental health counseling), medication or both.
- Psychotherapy. It may help to talk through your concerns with a psychiatrist, psychologist or other mental health provider. Through therapy, you can find better ways to cope with your feelings, solve problems, set realistic goals and respond to situations in a positive way. Sometimes family or relationship therapy also helps.
- Antidepressants. Your doctor may recommend an antidepressant. If you’re breast-feeding, any medication you take will enter your breast milk. However, some antidepressants can be used during breast-feeding with little risk of side effects for your baby. Work with your doctor to weigh the potential risks and benefits of specific antidepressants.
With appropriate treatment, postpartum depression usually goes away within six months. In some cases, postpartum depression lasts much longer, becoming chronic depression. It’s important to continue treatment after you begin to feel better. Stopping treatment too early may lead to a relapse.
Postpartum psychosis
Postpartum psychosis requires immediate treatment, often in the hospital. Treatment may include:
- Medication. When your safety is assured, a combination of medications — such as antidepressants, antipsychotic medications and mood stabilizers — may be used to control your signs and symptoms.
- Electroconvulsive therapy (ECT). If your postpartum depression is severe and does not respond to medication, ECT may be recommended. During ECT, a small amount of electrical current is applied to your brain to produce brain waves similar to those that occur during a seizure. The chemical changes triggered by the electrical currents can reduce the symptoms of psychosis and depression, especially when other treatments have failed.
Treatment for postpartum psychosis can challenge a mother’s ability to breast-feed. Separation from the baby makes breast-feeding difficult, and some medications used to treat postpartum psychosis aren’t recommended for women who are breast-feeding. If you’re experiencing postpartum psychosis, your doctor can help you work through these challenges.
Coping and support
The already stressful, exhausting period following a baby’s birth is more difficult when depression occurs. But remember, postpartum depression is never anyone’s fault. It’s a common medical condition that needs treatment.
So, if you’re having trouble coping with postpartum depression, talk with a therapist. Ask your doctor or therapist about local support groups for new moms or women who have postpartum depression.
The sooner you get help, the sooner you’ll be fully equipped to cope with depression and enjoy your new baby.
Prevention
If you have a history of depression — especially postpartum depression — tell your doctor if you’re planning on becoming pregnant or as soon as you find out you’re pregnant.
- During pregnancy, your doctor can monitor you closely for signs and symptoms of depression. He or she may have you complete a depression-screening questionnaire during your pregnancy and after delivery. Sometimes mild depression can be managed with support groups, counseling or other therapies. In other cases, antidepressants may be recommended — even during pregnancy.
- After your baby is born, your doctor may recommend an early postpartum checkup to screen for signs and symptoms of postpartum depression. The earlier it’s detected, the earlier treatment can begin. If you have a history of postpartum depression, your doctor may recommend antidepressant treatment or psychotherapy immediately after delivery.




Thank you for sharing this and your experience with it. I think it’s important that people know the symptoms and know they aren’t alone when dealing with this after having a baby. I think society makes new moms or mothers feel bad if they experience post partum depression.
LikeLiked by 1 person
Yes I agree with you . It is supposed to be the happiest day of our lives and sometimes it doesn’t turn out the way we always dreamed. Thank you for reading and for your great feedback I appreciate it.
LikeLike